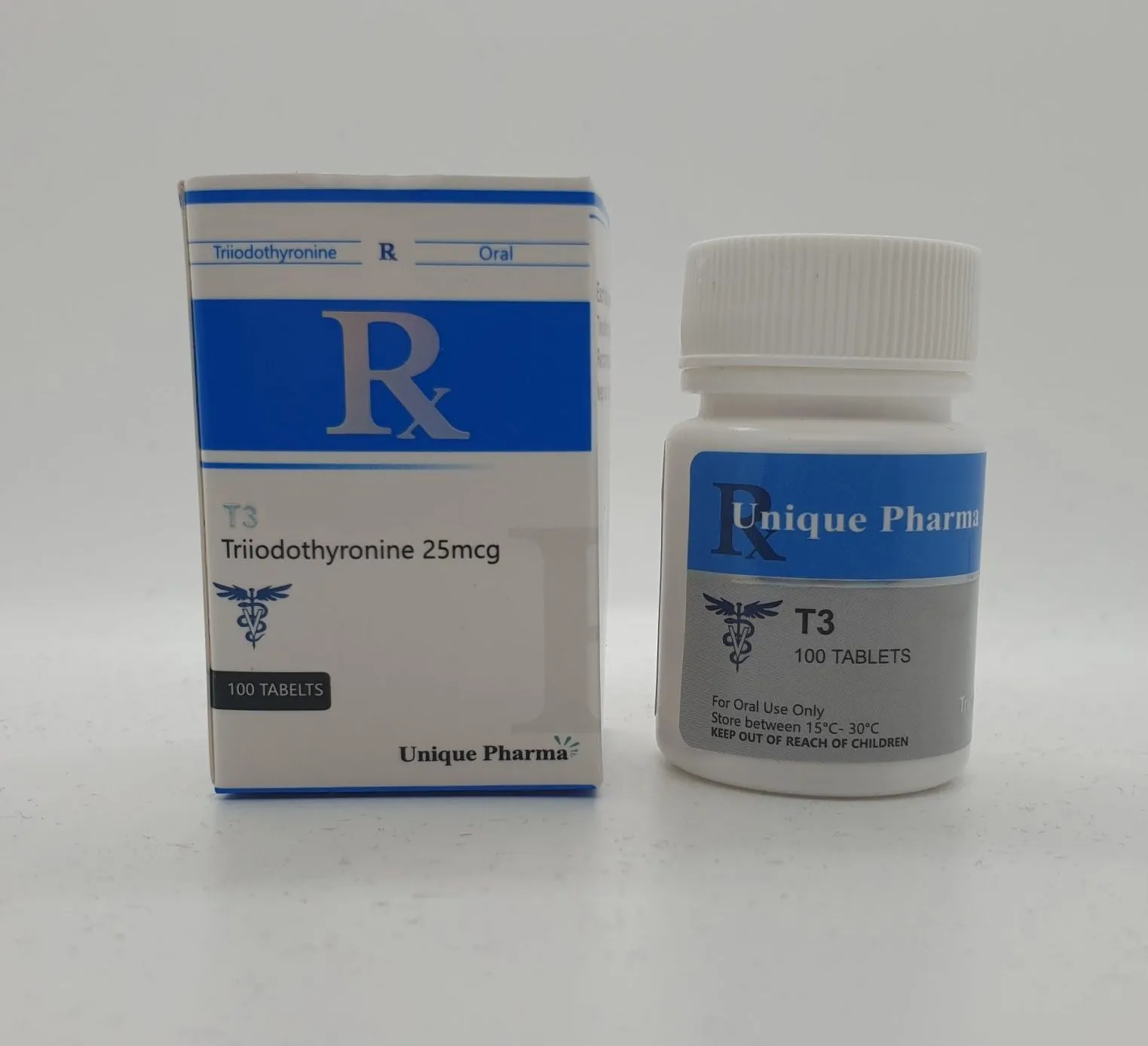
T3 Liothyronine (25 mcg) | Unique Pharma
€ 45,00
Auf LagerBuy premium T3 Liothyronine from Unique Pharma. Lab-tested, fast shipping, competitive prices. Effective for metabolic enhancement.
Akne
Yes
Halbwertszeit
9-12 Hours
Dosierung
20-40mg Daily
Nachweiszeit
5 Days
Aromatisierung
N/A
Wasserretention
No
Hepatotoxizität
N/A
HBR
N/A
Produktinformation
Über T3 Liothyronine (25 mcg) | Unique Pharma
Chemical Profile
- Generic name: Liothyronine Sodium (commonly known as T3)
- Chemical class: Synthetic thyroid hormone
- Molecular formula: C15H11I3NNaO4
- Molecular weight: approximately 672.96 g·mol−1
- Physical form: oral solid dosage (tablets)
- Terminal elimination half-life: approximately 2.5 days
Clinical Pharmacology
T3 (Liothyronine) is the active form of thyroid hormone that directly affects cellular metabolism. It increases basal metabolic rate, enhances protein synthesis, and promotes lipolysis. Unlike T4, T3 does not require conversion and acts directly on thyroid hormone receptors.
Applications
- Enhancement of metabolic rate during cutting phases
- Fat loss acceleration
- Maintenance of metabolic function during caloric restriction
- Synergistic use with anabolic compounds
Dosage Guidelines
Typical dosing starts at 25mcg daily and may be gradually increased. Maximum recommended doses vary but typically do not exceed 75-100mcg daily. Tapering protocols are essential to prevent thyroid suppression. Always consult with a healthcare professional before use.
1. Description: Clinical summary
"T3" refers to triiodothyronine (active thyroid hormone, chemical abbreviation T3). Clinically, liothyronine sodium is the pharmaceutical preparation of T3 used to treat certain thyroid-related disorders. T3 is the metabolically active thyroid hormone that increases basal metabolic rate, potentiates catecholamine effects, and regulates development and differentiation in many tissues.
Primary clinical uses
- Replacement or adjunctive therapy in hypothyroidism (less commonly used as sole long‑term replacement than levothyroxine/T4).
- Short‑term use when more rapid onset of action is desired.
- Treatment of severe, life‑threatening hypothyroidism (myxedema coma) as part of emergency management (often IV).
- Diagnostic uses historically (suppression/stimulation tests) but rarely used for this today.
General considerations
- T3 has a faster onset and shorter half‑life than T4 (levothyroxine). Because of this, it causes more rapid changes in serum thyroid hormone levels and clinical effect but also more fluctuation and higher risk of iatrogenic thyrotoxicosis if not carefully dosed.
- T4 (levothyroxine) is preferred for most chronic replacement because it is converted to T3 peripherally and provides steady levels. T3 may be used in selected patients (e.g., persistent symptoms despite normalized TSH on T4, need for rapid correction, or specific endocrinologist-directed combination therapy).
2. How does t3 work?: Mechanism of action
- T3 binds to nuclear thyroid hormone receptors (TRα and TRβ) in target tissues. The hormone‑receptor complex modulates transcription of thyroid‑responsive genes, affecting protein synthesis and metabolic activity.
- Effects at the cellular level include increased mitochondrial activity, upregulation of enzymes involved in carbohydrate and lipid metabolism, increased β‑adrenergic receptor expression (augmenting sensitivity to catecholamines), and modulation of cardiovascular function (increased heart rate and cardiac output).
- Compared with T4, T3 is the biologically active form and produces more immediate genomic and non‑genomic effects. Peripheral tissues normally convert T4 to T3 via deiodinases; pharmacologic T3 bypasses this conversion.
3. Dosage: Medical and varying usage guidelines
Important: Dosing must be individualized and supervised by a clinician. Monitor symptoms, heart rate, blood pressure and thyroid function tests (TSH; free T3/free T4 when appropriate). The following are common clinical regimens and typical ranges used in adults; institutional protocols and specialist recommendations should be followed.
Oral (liothyronine sodium)
- Typical adult replacement dosing:
- Starting dose for otherwise healthy adults: commonly 5–25 mcg once daily, titrating upward based on response and labs.
- Typical maintenance dose range: 25–75 mcg/day (often given once daily or divided into two doses to reduce peak symptoms).
- Elderly patients or those with coronary artery disease, arrhythmias, or other significant cardiac disease:
- Start very low (e.g., 5 mcg/day) and increase slowly (e.g., by 5 mcg increments every 1–3 weeks) with close cardiac monitoring.
- Combination therapy (levothyroxine + liothyronine):
- Some clinicians substitute a small dose of liothyronine for part of levothyroxine (e.g., replace a portion of T4 dose with T3 by weight-equivalence). Approximate potency conversions: 1 mcg T3 ≈ 3–4 mcg T4 — this is approximate only; any change should be made by an endocrinologist with biochemical monitoring and symptom assessment.
- Common combination regimens vary widely (e.g., 10–20 mcg T3 daily in divided doses combined with reduced T4), but approaches differ and evidence is mixed.
Intravenous (hospital, severe hypothyroidism/myxedema coma)
- IV liothyronine is used when enteral absorption is impaired or rapid correction is needed.
- Common regimens used in critical care settings (examples; follow institutional protocols):
- Loading bolus 5–10 mcg IV followed by continuous infusion of 2.5–10 mcg/hour OR
- Bolus 10–20 mcg IV followed by 1–2 mcg/hour infusion.
- Some centers use a single bolus followed by oral transition; others use different bolus sizes. Because of risk of cardiac complications, IV dosing should be performed under intensive monitoring and usually in conjunction with IV glucocorticoid administration until concomitant adrenal insufficiency is excluded.
- For myxedema coma, some guidelines recommend using levothyroxine (IV) or a combination of IV T4 + T3; local protocols vary.
Pediatric use
- Levothyroxine is the usual agent for congenital or chronic pediatric hypothyroidism. Liothyronine may be used in specific circumstances (e.g., certain testing or particular clinical scenarios) and dosing must be weight‑based and determined by pediatric endocrinology. Do not attempt to dose children with T3 without specialist input.
Off‑label and non‑medical use
- T3 has been misused for weight loss or athletic performance. This is unsafe and associated with serious cardiovascular and metabolic risks. Such use is not recommended.
Monitoring and adjustment
- When using T3, monitor heart rate and cardiac symptoms closely. Measure TSH and free thyroid hormone levels as clinically indicated. TSH may be suppressed disproportionately with exogenous T3; free T3 measurements are often useful when the drug is being used.
- Dose changes should be conservative in patients with cardiac risk, older adults, or long-standing hypothyroidism.
4. Side effects: Common and rare bad effects
Adverse effects generally reflect excess thyroid hormone (thyrotoxicosis) and are more likely if dosing is excessive or titration too rapid.
Common (dose‑related)
- Palpitations, tachycardia, increased pulse rate
- Nervousness, anxiety, irritability, tremor
- Heat intolerance, sweating
- Weight loss, increased appetite
- Insomnia
- Diarrhea, increased bowel movements
- Menstrual irregularities
- Muscle weakness
Cardiovascular and serious risks (can be life‑threatening)
- Arrhythmias (including atrial fibrillation)
- Worsening or precipitation of angina, myocardial ischemia or myocardial infarction, particularly in patients with known coronary artery disease
- Heart failure decompensation in susceptible individuals
Endocrine/metabolic
- Decreased bone mineral density and increased risk of osteoporosis (with chronic overtreatment)
- Unmasked or worsened adrenal insufficiency in patients with untreated secondary adrenal failure — adrenal status should be assessed prior to aggressive thyroid hormone replacement in some clinical contexts
Allergic/other
- Hypersensitivity reactions are uncommon but possible.
Rare but important
- Severe cardiac events (fatal arrhythmias, myocardial infarction) with inappropriate dosing or in vulnerable patients
- Acute adrenal crisis if adrenal insufficiency is unrecognized and thyroid hormone is given without glucocorticoid support in critical cases
- Severe neuropsychiatric manifestations (rare)
Drug interactions that increase adverse effects
- Concomitant sympathomimetics or catecholamines may potentiate cardiac effects.
- Warfarin anticoagulation may be potentiated (increased INR) as thyroid hormone increases catabolism of vitamin K‑dependent clotting factors; monitor INR and adjust anticoagulant dose.
- Drugs that alter absorption (e.g., bile acid sequestrants, calcium/iron supplements, proton pump inhibitors) or metabolism (amiodarone, propylthiouracil, beta‑blockers, certain enzyme inducers/inhibitors) may affect T3 levels or response.
If any signs of cardiac ischemia, new arrhythmia, severe tremor, or other severe symptoms occur, stop the drug and seek urgent medical care.
5. Storage: HOW to store it
- Keep the medication in its original container with label intact.
- Store at controlled room temperature, typically 15–30 °C (59–86 °F), unless the product labeling specifies otherwise.
- Protect from moisture and light; keep the container tightly closed.
- Keep out of reach of children and pets.
- Do not use past the expiration date printed on the packaging.
- For liquid formulations or hospital IV preparations, follow manufacturer or institutional pharmacy guidance about storage, dilution, and stability (e.g., discard opened vials per policy).
- Dispose of unused medication safely per local regulations or pharmacy take‑back programs.
Additional practical and safety notes
- Do not self‑adjust dose: changes should be guided by a clinician and laboratory monitoring.
- Before initiating T3 (especially at higher doses or IV), evaluate cardiac status and consider ECG monitoring in older patients or those with cardiac disease.
- In pregnancy, levothyroxine (T4) is generally preferred for replacement; if T3 is used, do so under specialist supervision with close monitoring.
- Keep a list of all medications and supplements and inform your clinician, since timing of doses relative to calcium, iron, or antacids affects absorption.
Summary
Liothyronine (T3) is the active thyroid hormone used medically for selected indications where rapid onset or specific effects are desired. It requires careful dosing, monitoring, and consideration of cardiovascular risk. Use should be guided by an endocrinologist or treating physician; inappropriate dosing or non‑medical use can cause serious harm.
1. Description
T3 refers to triiodothyronine (generic name: liothyronine sodium when used pharmaceutically), the active thyroid hormone containing three iodine atoms. It is a prescription medication used to treat hypothyroidism in selected situations, and it is used intravenously as part of emergency management of severe hypothyroid states (myxedema coma). Compared with levothyroxine (T4), T3 has a faster onset of action, shorter half-life, and greater immediate metabolic potency per microgram. T3 is indicated when rapid correction of hypothyroid symptoms is needed or when patients do not adequately convert T4 to T3, though levothyroxine (T4) remains the standard first-line therapy for most patients.
Clinical uses
- Primary hypothyroidism (selected patients or as adjunct to levothyroxine)
- Secondary/central hypothyroidism (occasionally, under specialist supervision)
- Myxedema coma (intravenous T3 as part of emergency therapy)
- Short-term use in diagnostic testing of thyroid function (rare)
Note: Use should be individualized and supervised by an endocrinologist or prescribing clinician because of cardiovascular and metabolic risks.
2. How does t3 work?
T3 is the biologically active thyroid hormone that binds to nuclear thyroid hormone receptors (TRα and TRβ) in target tissues. Once bound, T3 modulates gene transcription of proteins involved in:
- Basal metabolic rate (increasing oxygen consumption and heat production)
- Carbohydrate, lipid, and protein metabolism
- Cardiovascular system (increasing heart rate, contractility, and cardiac output)
- Thermoregulation and CNS function
Mechanistically, T3 enters cells (or is generated intracellularly from T4 by deiodinases), translocates to the nucleus, and alters transcription of genes with thyroid hormone response elements. Clinically, this results in increased metabolic activity, increased heart rate and contractility, and alterations in lipid and glucose metabolism.
Pharmacokinetics (general)
- Oral absorption: high but variable; peak serum levels within 2–4 hours.
- Half-life: substantially shorter than T4 (roughly 18–24 hours, variable by source); requires more frequent dosing or divided daily dosing.
- Onset: clinical effects often occur faster than with levothyroxine; symptomatic change may be noticed within days to weeks.
- Clearance: hepatic metabolism and deiodination.
3. Dosage
All dosing should be individualized according to age, weight, cardiac status, pregnancy, concomitant medications, and laboratory monitoring (TSH, free T4/T3 as appropriate). The following are general reference ranges and common regimens used in practice—use only under clinician direction.
Oral liothyronine (typical adult dosing)
- Initial (adults without cardiac disease): 5–25 mcg once daily. Many clinicians start at 5–10 mcg/day and increase in 5–10 mcg increments every 1–2 weeks based on symptoms and heart rate.
- Typical maintenance: 25–75 mcg/day, often given in divided doses (e.g., morning ± midday) due to short half-life.
- Upper limits: some patients are maintained at 75–100 mcg/day, but higher doses increase risk of thyrotoxicosis and cardiovascular adverse events; careful monitoring required.
Switching from levothyroxine to liothyronine or adding T3
- Conversion is approximate: 25 mcg liothyronine ≈ 100 mcg levothyroxine (approximate T4:T3 ratio ~4:1), but equivalence varies between patients. When converting, reduce total thyroid hormone dose appropriately and titrate using labs and symptoms.
- Combination therapy (T4 + T3): used by some patients and clinicians (e.g., small dose T3 added to T4). Common starting supplemental T3 doses are 5–10 mcg/day, often given in the morning; levothyroxine dose is reduced proportionally.
Pediatric dosing
- Levothyroxine is preferred in congenital hypothyroidism. Liothyronine is used rarely and only under specialist care.
- When used, dosing is weight- and age-dependent and must be determined by a pediatric endocrinologist.
Myxedema coma (severe hypothyroid emergency)
- IV regimens vary. Typical approaches:
- Initial IV bolus 5–20 mcg of liothyronine, followed by 2.5–10 mcg IV every 8 hours, titrated to response.
- Alternative regimens use an initial 10 mcg IV bolus then 10 mcg IV every 8 hours.
- Use in combination with IV glucocorticoids until concomitant adrenal insufficiency is excluded.
- Management should be in an intensive care setting with endocrine consultation and cardiac monitoring.
Special populations
- Elderly and patients with coronary artery disease: start at very low doses (e.g., 5 mcg/day) and titrate slowly; these patients are at higher risk for ischemia, arrhythmia, and myocardial infarction.
- Pregnancy: levothyroxine is generally preferred for hypothyroidism in pregnancy because of stable pharmacokinetics; if T3 is used, frequent monitoring and specialist management are required.
- Renal/hepatic impairment: monitor closely; dose adjustments may be needed.
Monitoring and titration
- Monitor symptoms, heart rate, blood pressure.
- Laboratory: TSH and free T4 are standard for titration with levothyroxine; when using T3 therapy, interpretation of TSH/free T4 may be altered—measure free T3 if clinically indicated. Frequent early monitoring (every 4–6 weeks when adjusting) is typical until stable.
- ECG and cardiac assessment in patients with known heart disease or when higher doses are used.
Cautions about off-label uses
- T3 has been misused for weight loss and performance enhancement. This is unsafe and associated with increased risk of arrhythmia, osteoporosis, and other complications. It should not be used for weight loss outside of a clear, supervised medical indication.
4. Side effects
Common and dose-related (typically related to excess thyroid hormone)
- Palpitations, tachycardia
- Nervousness, anxiety, tremor, insomnia
- Heat intolerance, sweating
- Increased appetite, weight loss
- Gastrointestinal upset
Cardiovascular and serious effects (more likely in overdose, elderly, or cardiac disease)
- Atrial or ventricular arrhythmias
- Exacerbation of angina pectoris, myocardial ischemia, myocardial infarction
- Heart failure exacerbation
Long-term risks when in supraphysiologic doses
- Accelerated bone loss and osteoporosis (increased fracture risk)
- Persistent tachycardia and cardiac stress
Rare but serious
- Thyroid storm (life‑threatening hyperthyroid state) if overdosed or in susceptible patients
- Severe allergic reactions (rare)
- Worsening of preexisting psychiatric illness (e.g., mania)
Drug interactions and clinical implications
- Anticoagulants (warfarin): thyroid hormone can increase sensitivity to warfarin → increased INR and bleeding risk; monitor INR and adjust warfarin dose.
- Sympathomimetics and adrenergic agents: additive cardiac stimulation.
- Amiodarone: can cause complex effects on thyroid function; coadministration requires close monitoring.
- Drugs that impair absorption: calcium, iron supplements, sucralfate, bile acid sequestrants—separate dosing times.
- Hepatic enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine) may increase thyroid hormone clearance → may require dose adjustment.
When to seek urgent care
- Rapid heart rate, chest pain, syncope, severe shortness of breath, high fever, or other signs suggesting arrhythmia, myocardial ischemia, or thyroid storm.
5. Storage
- Store liothyronine (oral tablets) at controlled room temperature, typically 20–25 °C (68–77 °F), with brief allowable excursions per product labeling. Avoid excessive heat.
- Protect from moisture and light. Keep in the original container with desiccant if provided.
- Do not store in the bathroom or near sinks where humidity is high.
- Keep out of reach of children and pets.
- For intravenous formulations: follow manufacturer instructions. Many lyophilized vials require reconstitution immediately before use; some prepared solutions have limited stability and may need refrigeration if not used immediately—follow the product insert for storage times and conditions.
- Dispose of unused or expired medication per local regulations; do not flush unless instructed.
Final notes
- T3 therapy requires individualized dosing and close clinical and laboratory monitoring due to its potency and cardiovascular effects. Levothyroxine (T4) remains first-line for most hypothyroid patients; use of T3 (liothyronine) should be guided by an experienced clinician. This document is educational and not a substitute for professional medical advice.
Dosierung
Empfohlen
20-40mg Daily
Halbwertszeit
9-12 Hours
Vorteile
- Laborgetestet auf Reinheit
- Pharmazeutische Qualität garantiert
- Diskreter und sicherer Versand
- Ausgezeichneter Kundenservice
- Schnelle Lieferung in ganz Europa
Kostenloser Versand
Kostenloser Versand bei Bestellungen über 200€.
Liefergarantie
Kostenloser Neuversand, wenn Ihre Bestellung nicht ankommt.
Schnelle Lieferung
Versand innerhalb 24h. Lieferung 48-72h in NL & BE.
Bitcoin Zahlung
Zahlen Sie sicher und bleiben Sie völlig anonym mit Bitcoin.
Sicherer Checkout
Gesicherte SSL-Verbindung für alle Transaktionen.
Authentisch
Echtheitsprüfung für alle unsere Produkte.